Connect With Us
Blog
Items filtered by date: September 2024
Recovering From an Ankle Injury

Recovering from a broken ankle requires patience and proper care to ensure the best possible outcome. The main goal is to allow the ankle to heal fully, which reduces the risk of chronic ankle problems. Some ankle fractures heal with rest and immobilization, while others may require surgery and the use of a brace. Following a podiatrist's guidance is essential for managing pain, reducing swelling, and beginning weight-bearing activities at the right time. This foot doctor will also provide exercises that help restore strength, mobility, and balance. Gradual return to daily activities is essential to avoid re-injury. Regular check-ins with a podiatrist can help monitor healing and address any complications, such as persistent pain or swelling. Long-term, some individuals may experience arthritis, but early treatment and careful rehabilitation can minimize this risk. If you are recovering from a broken ankle, it is suggested that you make an appointment with a podiatrist for treatment options.
Broken ankles need immediate treatment. If you are seeking treatment, contact one of our podiatrists from Florida Foot & Ankle Group, P.A.. Our doctors can provide the care you need to keep you pain-free and on your feet.
Broken Ankles
A broken ankle is experienced when a person fractures their tibia or fibula in the lower leg and ankle area. Both of these bones are attached at the bottom of the leg and combine to form what we know to be our ankle.
When a physician is referring to a break of the ankle, he or she is usually referring to a break in the area where the tibia and fibula are joined to create our ankle joint. Ankles are more prone to fractures because the ankle is an area that suffers a lot of pressure and stress. There are some obvious signs when a person experiences a fractured ankle, and the following symptoms may be present.
Symptoms of a Fractured Ankle
- Excessive pain when the area is touched or when any pressure is placed on the ankle
- Swelling around the area
- Bruising of the area
- Area appears to be deformed
If you suspect an ankle fracture, it is recommended to seek treatment as soon as possible. The sooner you have your podiatrist diagnose the fracture, the quicker you’ll be on the way towards recovery.
If you have any questions, please feel free to contact one of our offices located in Debary, Lake Mary, Orlando, and Oviedo, FL . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Pain in the Top of the Foot

Pain in the top of the foot can arise from various causes, often linked to issues with tendons, ligaments, or bones. Common conditions include extensor tendinitis, where the tendons that lift the toes become inflamed, or stress fractures from overuse or repetitive strain. Other potential causes include nerve compression, such as from wearing tight footwear or a condition like Morton's neuroma, and arthritis affecting the foot joints. Bruises or injuries can also lead to localized pain on top of the foot. Proper diagnosis is imperative for effective treatment, which may involve rest or changes in footwear. If you are experiencing persistent or severe foot pain, it is suggested that you consult a podiatrist for a proper diagnosis and treatment.
Foot Pain
Foot pain can be extremely painful and debilitating. If you have a foot pain, consult with one of our podiatrists from Florida Foot & Ankle Group, P.A.. Our doctors will assess your condition and provide you with quality foot and ankle treatment.
Causes
Foot pain is a very broad condition that could be caused by one or more ailments. The most common include:
- Bunions
- Hammertoes
- Plantar Fasciitis
- Bone Spurs
- Corns
- Tarsal Tunnel Syndrome
- Ingrown Toenails
- Arthritis (such as Gout, Rheumatoid, and Osteoarthritis)
- Flat Feet
- Injury (from stress fractures, broken toe, foot, ankle, Achilles tendon ruptures, and sprains)
- And more
Diagnosis
To figure out the cause of foot pain, podiatrists utilize several different methods. This can range from simple visual inspections and sensation tests to X-rays and MRI scans. Prior medical history, family medical history, and any recent physical traumatic events will all be taken into consideration for a proper diagnosis.
Treatment
Treatment depends upon the cause of the foot pain. Whether it is resting, staying off the foot, or having surgery; podiatrists have a number of treatment options available for foot pain.
If you have any questions, please feel free to contact one of our offices located in Debary, Lake Mary, Orlando, and Oviedo, FL . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Non-Diabetic Foot Ulcers
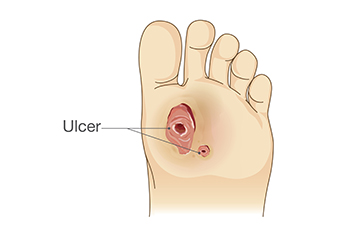
Non-diabetic foot ulcers are open sores or wounds that occur on the feet, typically due to poor circulation, pressure, or injury. Unlike diabetic ulcers, these wounds are not directly caused by high blood sugar levels, but can still lead to severe complications if left untreated. These ulcers often develop from pressure points on the feet, especially in individuals with limited mobility or poor blood flow. Risk factors include age, obesity, peripheral artery disease, and wearing ill-fitting shoes. Recognizing a foot ulcer early is important. Look for persistent redness, swelling, and an open sore that does not heal. To prevent these ulcers, regularly inspect your feet, wear appropriate footwear, and manage any underlying conditions that affect circulation. Treatment involves cleaning the wound, relieving pressure with specialized footwear, and possibly using topical medications. If you notice you have developed a foot ulcer, it is suggested that you visit a podiatrist who can assess the ulcer's severity, provide targeted treatments, and suggest preventive strategies to avoid recurrence, ensuring optimal foot health.
Wound care is an important part in dealing with diabetes. If you have diabetes and a foot wound or would like more information about wound care for diabetics, consult with one of our podiatrists from Florida Foot & Ankle Group, P.A.. Our doctors will assess your condition and provide you with quality foot and ankle treatment.
What Is Wound Care?
Wound care is the practice of taking proper care of a wound. This can range from the smallest to the largest of wounds. While everyone can benefit from proper wound care, it is much more important for diabetics. Diabetics often suffer from poor blood circulation which causes wounds to heal much slower than they would in a non-diabetic.
What Is the Importance of Wound Care?
While it may not seem apparent with small ulcers on the foot, for diabetics, any size ulcer can become infected. Diabetics often also suffer from neuropathy, or nerve loss. This means they might not even feel when they have an ulcer on their foot. If the wound becomes severely infected, amputation may be necessary. Therefore, it is of the upmost importance to properly care for any and all foot wounds.
How to Care for Wounds
The best way to care for foot wounds is to prevent them. For diabetics, this means daily inspections of the feet for any signs of abnormalities or ulcers. It is also recommended to see a podiatrist several times a year for a foot inspection. If you do have an ulcer, run the wound under water to clear dirt from the wound; then apply antibiotic ointment to the wound and cover with a bandage. Bandages should be changed daily and keeping pressure off the wound is smart. It is advised to see a podiatrist, who can keep an eye on it.
If you have any questions, please feel free to contact one of our offices located in Debary, Lake Mary, Orlando, and Oviedo, FL . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Risk Factors and Causes of Cracked Heels

Cracked heels, a common foot condition, often result from various risk factors and underlying causes. Dry skin is a primary contributor, often worsened by prolonged standing on hard surfaces. People with diabetes or other conditions affecting blood circulation are at increased risk of cracked heels. Wearing open-backed shoes, flip-flops, or high heels can place undue pressure on the heels, leading to cracks and fissures. Environmental factors, such as low humidity, can also strip moisture from the skin, making it more prone to cracking. Additionally, obesity adds extra weight, which can put additional stress on the heels. Regular moisturizing and wearing supportive, well-fitting footwear can help prevent and manage cracked heels. If you have cracked heels, it is suggested that you visit a podiatrist for treatment, which may include prescribed medication.
Cracked heels are unsightly and can cause further damage to your shoes and feet. If you have any concerns, contact one of our podiatrists from Florida Foot & Ankle Group, P.A.. Our doctors can provide the care you need to keep you pain-free and on your feet.
Cracked Heels
Cracked heels appear unappealing and can make it harder for you walk around in sandals. Aside from looking unpleasant, cracked heels can also tear stockings, socks, and wear out your shoes. There are several methods to help restore a cracked heel and prevent further damage.
How Do You Get Them?
Dry skin is the number one culprit in creating cracked heels. Many athletes, walkers, joggers, and even swimmers suffer from cracked heels. Age and skin oil production play a role to getting cracked heels as well.
Promote Healing
Over the counter medicines can help, especially for those that need instant relief or who suffer from chronic dry feet.
Wear Socks – Wearing socks with medicated creams helps lock in moisture.
Moisturizers – Applying both day and night will help alleviate dryness which causes cracking.
Pumice Stones – These exfoliate and remove dead skin, which allows for smoother moisturizer application and better absorption into the skin.
Change in Diet
Eating healthy with a well-balanced diet will give the skin a fresh and radiant look. Your body responds to the kinds of food you ingest. Omega-3 fatty acids and zinc supplements can also revitalize skin tissue.
Most importantly, seek professional help if unsure how to proceed in treating cracked heels. A podiatrist will help you with any questions or information needed.
If you have any questions, please feel free to contact one of our offices located in Debary, Lake Mary, Orlando, and Oviedo, FL . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Blog Archives
- March 2025
- February 2025
- January 2025
- December 2024
- November 2024
- October 2024
- September 2024
- August 2024
- July 2024
- June 2024
- May 2024
- April 2024
- March 2024
- February 2024
- January 2024
- December 2023
- June 2023
- May 2023
- April 2023
- March 2023
- February 2023
- January 2023
- December 2022
- November 2022
- October 2022
- September 2022
- August 2022
- July 2022
- June 2022
- April 2022
- March 2022
- February 2022
- January 2022
- December 2021
- November 2021
- October 2021
- September 2021
- August 2021
- July 2021
- June 2021
- May 2021
- April 2021
- March 2021
- February 2021
- January 2021
- December 2020
- November 2020
- October 2020
- September 2020
- August 2020
- July 2020
- June 2020
- May 2020
- April 2020
- March 2020
- February 2020
- January 2020
- December 2019
- November 2019
- October 2019
- September 2019
- August 2019
- July 2019
- June 2019
- May 2019
- April 2019
- March 2019
- February 2019
- January 2019
- December 2018
- November 2018
- October 2018
- September 2018
- August 2018
- July 2018
- June 2018
- May 2018
- April 2018
- March 2018
- February 2018
- January 2018
